 Understanding pain is one of the biggest problems facing conventional western medicine. According to the CDC, an estimated 50 million adults suffered from chronic pain in 2016. Because the experience of pain is subjective, there is no easy way to accurately measure pain, or the treatment of it. In this article, trainer Sean O’Hara takes a look at the phenomenon of pain: the difference between chronic and acute pain, and how safe exercise can help break the cycle of chronic pain.
Understanding pain is one of the biggest problems facing conventional western medicine. According to the CDC, an estimated 50 million adults suffered from chronic pain in 2016. Because the experience of pain is subjective, there is no easy way to accurately measure pain, or the treatment of it. In this article, trainer Sean O’Hara takes a look at the phenomenon of pain: the difference between chronic and acute pain, and how safe exercise can help break the cycle of chronic pain.
What is it?
Pain is defined as localized physical suffering associated with bodily disorder, leading to evasive action. Pain falls into two categories, acute and chronic. At the most basic level, pain is the sensation we feel when neurons called nociceptors are activated in response to extreme temperature, pressure, or injury-producing chemicals. As the nociceptor relays this information to the brain, we feel pain as a way of our brain telling us that something is harming us. Pain serves a vital function by making us aware of threats. When tissue becomes damaged by a threat, pain will be present until healing occurs. Pain associated with tissue damage usually resolves within 12 weeks, and is known as acute pain.
The Difference Between Chronic and Acute Pain
When a pain-free state is not restored in a reasonable period of time, typically 12 weeks, the pain condition becomes chronic. This marks the point when the pain cannot be understood solely through the mechanism of nociception. Chronic pain is far more difficult to make sense of because the underlying causes escape our intuitions. Despite decades of research, chronic pain remains poorly understood and notoriously hard to control. One recent study showed that even comprehensive treatment with painkilling prescription drugs helps, on average, only about 58% of people with chronic pain.
For those with chronic pain, something additional is happening within the person’s nervous system that causes a persistence of pain. Neuroscience researcher Alexander Ploghaus discovered that when pain persists it causes an increased sensitivity in two parts of the nervous system, at the site of injury (nerve sensitization) and in the brain (central sensitization) where pain is evoked (pain experience). Neurons with increased sensitivity are more active at lower levels of threat. In chronic cases, tissue healing occurs and at the same time neuronal sensitivity increases, creating the conditions for an individual to sense pain with healed tissues. Pain can then persist without any of the initial tissue damage. This physiological state leads lead to a cycle that drives increased inflammation in the body, continually triggering the sensitised neurons to create a pain experience. Without breaking this cycle, chronic pain cannot be resolved.
Strength Training’s Effect on Chronic Pain
For those suffering for months and years, it can become challenging to motivate ourselves to move when our body is telling us to stay still. Even a small program can seem overwhelming, because our instinct is to avoid movement to protect ourselves from more pain. This makes sense in the initial stages of a healing process when the injured tissues benefit from immobilization but when it makes us stagnant and sedentary it can have the inverse effect.
This phenomenon is well highlighted by the effects we see on astronauts who spend extended periods of time in a reduced gravity. This environment, outer space, takes resistance off the body. The research currently shows that the back pain astronauts experience in space and thereafter is caused by muscle atrophy in the muscles that stabilize the spine. To help mitigate this problem, astronauts exercise vigorously everyday to maintain muscle mass and strength.
The effects of a sedentary lifestyle on our nervous system is similar to the effects of the reduced gravitational environment of space, our muscles atrophy, weaken, and begin to struggle supporting our skeleton. Over time, these deleterious effects of inactivity and limited resistance on our bodies can develop into similar chronic pain conditions. Daily or weekly movement, exercise, and strength training can help to reverse or slow down these effects.
Getting Started
The following movements are generally safe, and can be helpful in reducing back pain and breaking the chronic pain cycle.
Table Top Rock Back
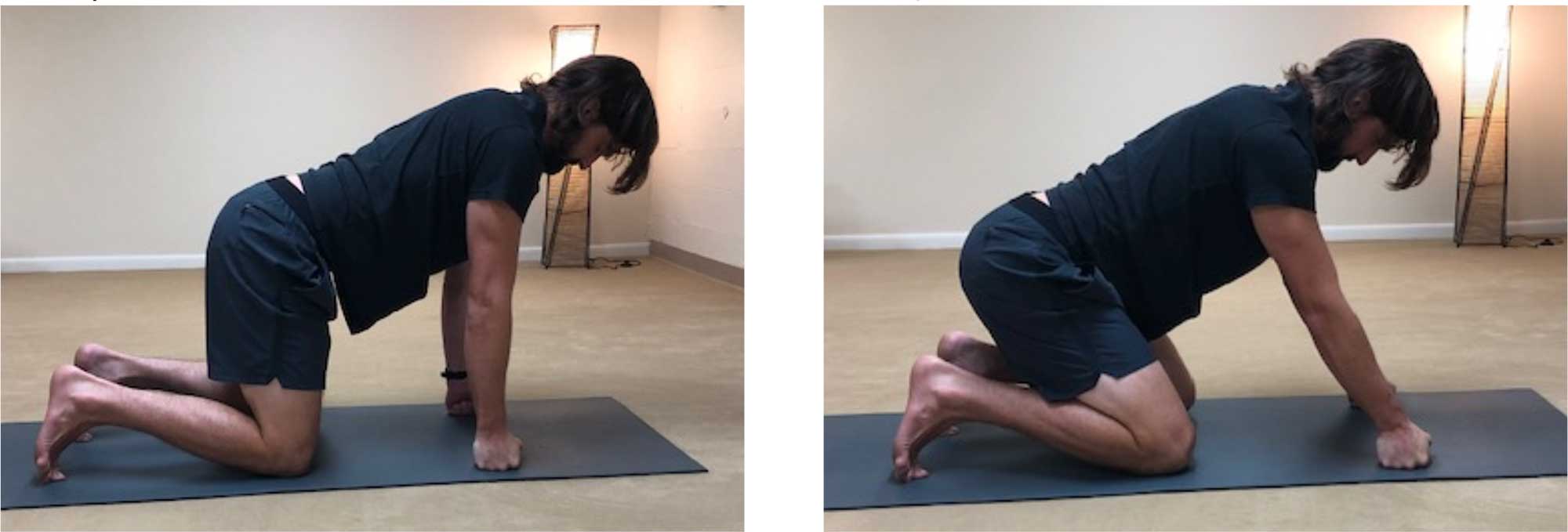
3 sets of 5 slow, mindful reps.
Plank—3 sets of 30 seconds/side

3 sets of 30 second holds.
Bird-dog

3 sets of 5 reps, with a 5 second hold.
References
Dublin, A., Patapoutian, A., Nociceptors: the sensors of the pain pathway. Journal of Clinical Investigation. 2010 Nov 1;120(11). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2964977/#idm139731546913664title
Twilley, N., The Neuroscience of Pain: the neural patterns behind pain’s infinite variety. The New Yorker Magazine, 2018, July 2, https://www.newyorker.com/magazine/2018/07/02/the-neuroscience-of-pain
Rainville J., Hartigan C., Martinez E., Linke J., Jouve C., Finn M., Exercise as an intervention for low back pain. Spine Journal. 2004 Jan-Feb(1):106-15. https://www.ncbi.nlm.nih.gov/pubmed/14749199
Green L.J., Moore A.R., Smith B.H., Physical activity and exercise from chronic pain in adults: an overview of Cochrane Reviews. The Cochrance Database of Dystemic Rev. 2017 Apr;2017(4):CD011279. https://www.ncbi.nlm.nih.gov/pmc/articles
Bailey JF., et al, From the international space station to the clinic: how prolonged unloading may disrupt lumbar spine stability. Spine Journal. 2018 Jan 18:7-14 https://www.ncbi.nlm.nih.gov/pubmed/28962911